|
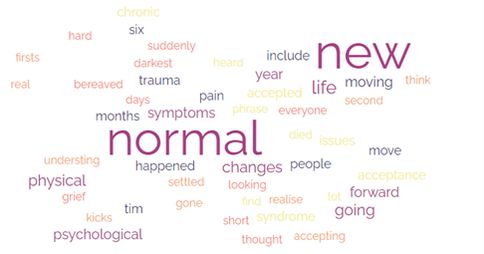
After Tim died, I heard the phrase ‘the new normal’ a lot. That I would find my ‘new normal’. That people settled into their ‘new normal’. That the ‘new normal’ kicks in after six months when you realise that it’s all real, or in the second year when all the firsts are over. But what is the new normal?
I think it’s about understanding the changes that we have gone through, accepting what has happened, and looking at how we move forward. This is about how it’s happened for me. It’s not the same for everyone, and for people in the darkest days of grief, the thought of a new normal may be too hard. The new normal: Physical and psychological The trauma of being bereaved, whether it’s suddenly or after a short or long illness, changes us physically and psychologically. Physical symptoms include headaches, chest pain, muscle and joint aches, sleep issues and immune system issues. Psychological changes include brain fog, flashbacks, panic attacks, dissociation and hyperarousal. Trauma also increases the risk of self-harm and suicidal feelings, and of irritable bowel syndrome (IBS), fibromyalgia and chronic pain, and chronic fatigue syndrome (CFS/ME). These changes don’t always last forever – for me, the physical symptoms eased after six months or a year, and the worst of the psychological symptoms after a year or two. It’s important that we look after ourselves, and this isn’t about fluffiness and bubble baths. It’s about genuinely being kind to ourselves, and about taking proper care of our mental and physical health. The new normal: Acceptance The new normal can be about acceptance, and this was significant for me. I accepted that this was my life now. That things were never going to be the same again. For a while it was just about keeping going, and putting one foot in front of the other. The next phase was reclaiming a space and a life for myself – I cleared and redecorated, I went back to university, I started The Widow’s Handbook. I accepted that grieving was a long-term thing. That I wasn’t going to ‘get over it’, or ‘move on’. That it was something that I was going to walk alongside. I also gave myself permission to feel happy again. The new normal: Moving forward Ever since I saw this brilliant TED talk from Nora McInerny, I have talked about ‘moving forward’ not ‘moving on’, because I have taken Tim with me into my new life. While it’s not the life I expected or planned for, it’s the life I have and it’s a life I like.
0 Comments
There isn't much information on the issues associated with the combination of grief and the menopause. So this is going to be rather shorter than I hoped it would be. The symptoms of the menopause, such as lack of sleep, loss of self-confidence, low mood, anxiety, brain fog, weight changes, emotional overload, exhaustion and flare ups in other health conditions, can overlap with many of the experiences in grief and blur in together. This can make it harder to work out what is grief and what is the menopause and makes both feel worse. The stress associated with grief may also worsen menopause symptoms, and there is a possibility that stress could even bring on an earlier menopause. There can be grief associated with the menopause itself, which could complicate the grief of bereavement. Menopause can bring up thoughts of the loss of youth and of aging, which may trigger grief about the loss of a partner.
For people who are grieving, the menopause can highlight the secondary loss of the chance of conceiving and carrying a baby. This can be especially hard for those who were trying for children at the time of their partner's death. The menopause also comes at a time where people may be caring for aging parents, or grieving their loss and missing their support. The fact that the symptoms of perimenopause and menopause and the symptoms of grief are so hard to separate may also mean that women (and trans and non-binary people) don't seek help for menopausal symptoms at what is already a difficult and overwhelming time. Coping with grief and the menopause Like grief, there is no one solution to the menopause. Be aware that the menopause may be masking or adding to your grief symptoms and be gentle with yourself. If you are struggling with the menopause talk to your doctor – there are options that can help you deal with the physical and psychological symptoms. Grief is bad enough without the menopause making it worse. HRT can help with some symptoms (I have just started with HRT patches to see if they can help with my fluctuating body temperature and disturbed sleep). The Menopause Charity's website has information, news and expert advice, and the NHS website has a section on 'Things you can do'. When Tim died it hurt. And I don't just mean that my heart broke. I mean that I hurt physically. I felt so tired that my bones ached. My stomach hurt. I felt sick. My head ached. I didn't experience this, but I know that other widows had chest pains so bad they ended up in A&E. And there's widow brain too. It's all completely normal with the shock and sadness that comes along with bereavement.
Please remember, though – if any of these symptoms become distressing, last a long time or get worse, please talk to your doctor, call 111, or in an emergency, call 999. Being exhausted Grief messes with our sleep, gives our brains a lot to do, stops us eating properly – it's hardly surprising it leaves us exhausted. Try to eat as well as you can, sleep when you can and manage your energy. Feeling pain in muscles and joints The tension of grief can leave us with aches and pains, and grief can actually make pain worse. Try to exercise if you can – even just a walk round the block – as exercise can improve mood. Try having a massage, which can also help skin hunger. Colleges that run health and beauty courses often have low-cost massages to provide experience for students. Chest pain and shortness of breath Chest pain and shortness of breath are associated with anxiety. However, if these come on suddenly or are painful, talk to your doctor of call 999 – paramedics and doctors would rather be called in for something that isn't serious that miss something that really is. Headaches Headaches often accompany anxiety and stress. Trying to relax can help, but it's easier said that done. Warm baths and music helped me. Widow brain The confusion, forgetfulness and lack of concentration that comes alongside bereavement is often known as widow brain. Stomach upsets and appetite changes Grief can make us eat more, eat less, eat junk food, comfort eat feel sick, feel hungry, think we are never going to feel hungry again. This is all normal and will settle. Try and eat some fruit and veg, but eat what makes you feel comforted. Picking up bugs Grief can affect our immune systems, leaving us more vulnerable to infection. Wash your hands regularly, make sure kitchen surfaces are clean, cook food thoroughly, get the vaccines you are offered, and wear a mask in crowded palaces during cold and flu season can help to keep infection levels down. Health anxiety One of the issues with the physical symptoms around grief is that they can become part of health anxiety, where we become convinced that every symptom, from a headache to a painful toe, is something life-changing. I have gastritis, and sometimes when its bad I vomit. I threw up blood one day. My wonderful GP, who was an incredible support to me after Tim died, fast-tracked me for an endoscopy while reassuring me that she was sure everything was okay, and fortunately she was right. On the flip side, bereavement can also leave us caring less about our health and ignoring symptoms. If you are on regular medications, keep taking them (pill boxes and reminders on phones are really helpful) and build in a bit of self care. |
AuthorI was widowed at 50 when Tim, who I expected would be my happy-ever-after following a marriage break-up, died suddenly from heart failure linked to his type 2 diabetes. Though we'd known each other since our early 20s, we'd been married less than ten years. Archives
July 2024
Categories
All
|




 RSS Feed
RSS Feed